What Is Cell Therapy for Cancer?
Cell therapy — also known as adoptive cell therapy — uses patients’ immune cells or those from a donor to identify and destroy cancer. Unlike traditional cancer treatments that affect cancerous and healthy cells, cell therapy focuses on cancer cells only. For instance, chemotherapy targets fast-growing cells throughout the body with powerful drugs. Radiation delivers high-energy particles to specific areas, damaging cancerous and healthy cells alike. Likewise, checkpoint inhibitors put a brake on the immune system to help T cells recognize and attack cancer, but they don’t add new immune cells to the body.
By contrast, cell therapy offers a more direct and personalized approach to cancer treatment, demonstrating long-lasting remission in some patients, including cases where standard therapies failed. It involves collecting T cells from patients or a matched donor and then engineering or multiplying the cells in a lab. Doctors then reintroduce the enhanced cells into the patient, where they seek out and destroy cancer cells with greater precision, reducing harm to healthy cells during treatment. This method boosts immune targeting and may also create long-term immune system memory against cancer. Some types of cell therapies used in cancer treatment include:
- CAR-T cell therapy: This treatment engineers patients’ T cells to recognize cancer cells via synthetic receptors. According to the National Cancer Institute, it has shown promising results in those suffering from blood cancers.
- Tumor-infiltrating lymphocytes: This treatment uses certain types of cells in your immune system that are already present in the tumor. Doctors remove, expand and strengthen these cells and then return them to the tumor to better attack cancer cells.
- Bria-IMT™: This cell therapy for advanced breast cancer uses premade genetically altered cancer cells to stimulate a patient’s immune system against their cancer. Because it doesn’t require collecting or modifying cells, it’s faster to administer and easier to access.
Bria-OTS™: This next-generation off-the-shelf platform from BriaCell offers a scalable solution to cancer treatment by matching patients’ cells with the most common HLA types. These ready-to-use cell lines create personalized treatments without the delays and expense of custom cell engineering.
What is BriaCell’s Cancer Therapy?
How Bria-IMT™ and Bria-OTS™ Destroy Cancer Cells
The mechanism of action of Bria-IMT™/Bria-OTS™ is currently under investigation.
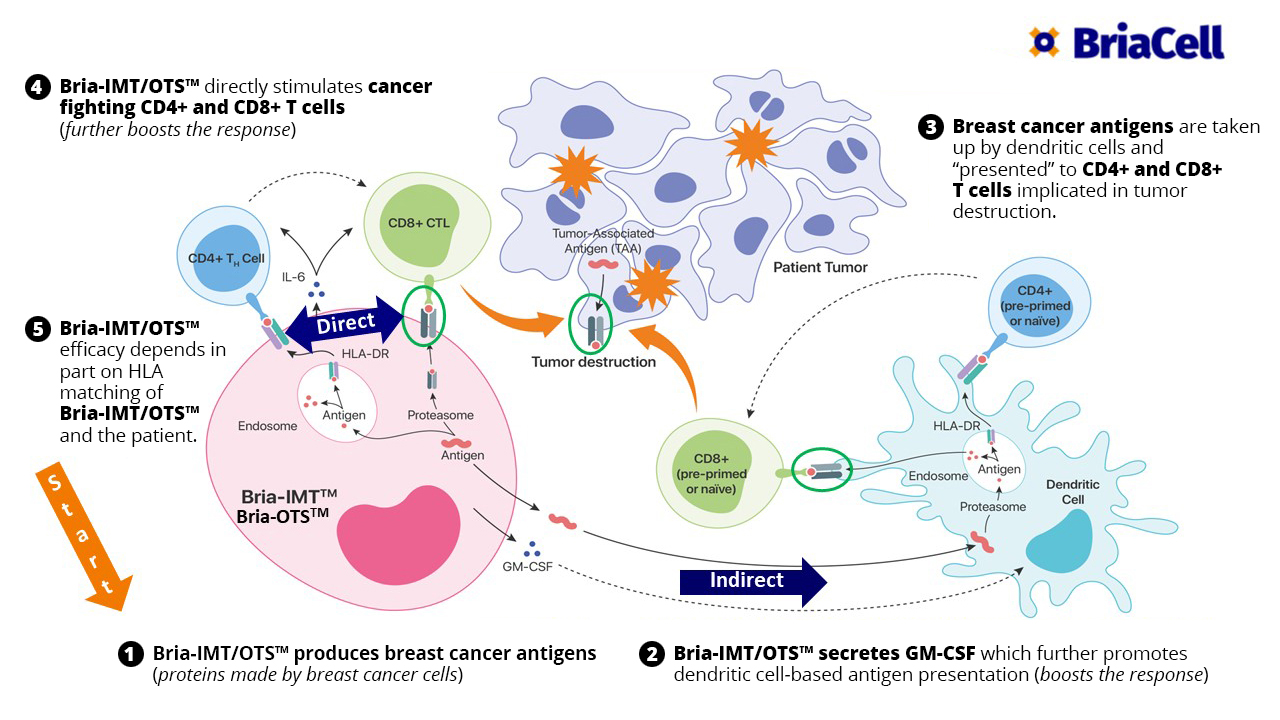
We believe that Bria-IMT™/Bria-OTS™, activates the patient’s immune system to recognize tumor cells and destroy them. We hypothesize that Bria-IMT™/Bria-OTS™, exert their action by stimulating the antigen-presentation system (i.e. the system that presents antigen material on the surface of the tumor cells) – to be recognized by the T cells of the immune system. Specifically, Bria-IMT™/Bria-OTS™, may stimulate the dendritic cells, a key component of the antigen-presenting system, to display certain immunogenic (i.e., immune response-generating) protein fragments to T cells, which activates the T cells to destroy the tumor cells either directly, or by inducing antibodies to the tumor cells. In addition, we also have shown that Bria-IMT™ is capable of directly stimulating cancer-fighting T cells. This further boosts the immune response against the tumor cells and enhances anti-cancer activity.
Our preliminary analyses have shown several up-regulated genes in Bria-IMT™ that encode proteins known to be immunogenic (i.e. immune response-generating), suggesting that Bria-IMT™ can stimulate the immune system against the cancer cells.
Bria-IMT™ is a human breast cancer cell line which expresses Her2/neu (a protein well known for its overexpression in breast cancer but also present on other epithelial malignancies including ovarian, pancreatic, colon, bladder and prostate cancers).
Bria-IMT™ has been engineered to produce and secrete granulocyte-macrophage-colony stimulating factor (GM-CSF), a protein that promotes dendritic cell function, a key component of the immune system, and hence activates the immune system.
Bria-IMT™ & Bria-OTS™
Potential Mechanisms of Specific Immune Activation in Advanced Metastatic Breast Cancer
- Bria-IMT/OTS™ produces breast cancer antigens (proteins made by breast cancer cells).
- Bria-IMT/OTS™ secretes GM-CSF which further promotes dendritic cell-based antigen presentation (boosts the response).
- Breast cancer antigens are taken up by dendritic cells and “presented” to CD4+ and CD8+ T cells implicated in tumor destruction.
- Bria-IMT/OTS™ directly stimulates cancer fighting CD4+ and CD8+ T cells (further boosts the response).
- Bria-IMT/OTS™ efficacy depends in part on HLA matching of Bria-IMT/OTS™ and the patient.
How BriaCell’s Cell Therapy Is Different
BriaCell takes a bold approach to cancer immunotherapy with its proprietary cell-based platforms: Bria-IMT and Bria-OTS. Our platforms offer a more accessible approach to cell therapy for cancer than most other treatments, thanks to their blend of personalization and practicality. By combining immunological precision with speed and scalability, we provide a highly targeted, patient-centered treatment that’s faster and more feasible to administer than traditional autologous cell therapies.
Our Bria-IMT and Bria-OTS treatments are allogenic (derived from cancer cell lines that are irradiated so they can’t proliferate), enabling patients to benefit from personalized cell-based immunotherapy without the hassle or expense of patient-specific harvesting. This HLA-matched cell therapy teams up donor cells with patients’ human leukocyte antigen type to stimulate an immune response, making treatment faster and easier to deploy and scale. This treatment works seamlessly with checkpoint inhibitors for an off-the-shelf cancer immunotherapy with enhanced efficacy, especially in resistant cancers.
Why Cell Therapy Matters in Cancer Care
Cell therapies are gaining more attention for several reasons, including greater precision in treatment. These therapies target cancer with more accuracy than traditional therapies because they utilize engineered or matched immune cells. Some patients experience long-lasting remissions after cell therapy, even after other therapies stopped working. Also, cell therapy has fewer side effects due to how it focuses only on cancerous cells and not healthy ones. Because cell therapy doesn’t damage healthy cells, patients generally stay healthier during treatment and beyond.
According to a 2023 article from Nature Reviews Clinical Oncology, adoptive cell therapies can induce prolonged remissions in patients with B cell malignancies with minimal long-term toxicities, and they often prove curative to a subset of patients. Likewise, in BriaCell’s clinical trials, patients with metastatic breast cancer who were treated with Bria-IMT plus a checkpoint inhibitor lived for more months than other similar patients reported in the literature. Additionally, Bria-OTS resolved a lung metastasis in a patient within 2 months of monotherapy with no observed toxicity. These results underscore the significant clinical success of adoptive cell therapies for certain types of cancer.